
The macula is the central region of the retina located in the back of the eye. The retina is analogous to the film of a camera that captures an image. The retina contains a dense array of cells called photoreceptors that sense light and initiate signals to the brain to process visual information. The macula is responsible for our central vision including reading, writing, color vision and recognizing faces.
The macula, just like any other part of the body, is subject to disease. For example, the macula can be swollen, wrinkled, or damaged by trauma. Systemic conditions such as diabetes and high blood pressure can damage the small blood vessels that supply the retina.
The most common disease of the macula is age-related macular degeneration (AMD). AMD is a common condition in people age 50 years and older and is the leading cause of visual disability in individuals over age 65.
People suffering from AMD may experience blurriness and distortion in their central vision. For example, patients may note that lines appear wavy or letters are missing on a printed page. However, many people with AMD have no visual symptoms and may retain 20/20 vision indefinitely. A relatively small percentage of people will lose central vision and the ability to read and drive a car. Although AMD can cause central vision loss, it does not typically lead to complete blindness.
Dry AMD is more common, and accounts for 90% of all cases. Dry AMD is identified during an eye examination by the presence of drusen, which are small whitish-yellow deposits under the retina. These drusen can disturb the light-sensing cells of the retina.
Dry AMD is often asymptomatic but symptoms may include gradual loss of central vision, blurry or distorted vision, or blank spots in the vision. In some patients dry AMD will advance to central vision loss due to geographic atrophy which is the loss of the pigmented cellular layer under the macula. The treatment of geographic atrophy is an active area of research as there are currently no effective therapies.
Dry AMD is monitored closely as it can potentially convert to the more severe type called wet AMD. Your doctor will determine the frequency of examinations needed to monitor your condition.
Wet AMD is caused by the growth of new, fragile blood vessels that develop as the eye attempts to repair the damage of macular degeneration. However, these fragile blood vessels are more harmful than helpful and can leak and bleed leading to damage to the macula. Over time, scarring can develop which permanently impairs central vision. Medications that block the growth of these blood vessels can be injected into the eye by a retina specialist to stop further progression and vision loss.

Macular degeneration can only be detected by having a complete dilated eye examination. If you are 60 or older or have a family member that has been diagnosed with macular degeneration, it is important to have your eyes checked yearly. With earlier detection, there is a better chance of maintaining vision.
The most significant risk factors for AMD are genetics (family history) and smoking. If you have a direct family member (mother, father, sister, brother) with AMD your risk for the disease is increased compared to the general population. If you are a smoker, your risk is more than 2 times greater compared to non-smokers.
Complete and comprehensive ophthalmic evaluation is important in the assessment of AMD. On a visit to a retina specialist, you will receive vision testing, eye drops to dilate the pupils and a complete examination of the front and back of the eye. Pupillary dilation may create near vision blurring and therefore, it may be helpful to have a driver accompany the patient, although this is not always required.
The Age Related Eye Disease Study (AREDS) demonstrated that a specific formulation of antioxidant vitamins and minerals can modestly lower the risk of progression of dry AMD to more advanced stages of AMD associated with vision loss.
This formulation is available over the counter from several different manufacturers. It is important to check with your medical doctor before starting the AREDS 2 supplement. Of note, smokers should avoid any supplementation with Beta-carotene (included in the original AREDS formulation but not in AREDS 2) due to an increased risk of lung cancer.
The prognosis for patients with wet AMD has improved considerably over the last decade with the advent of new pharmacologic therapies. There are now three different medications used by retina specialists to block the growth of new and leaking blood vessels. These medications inhibit Vascular Endothelial Growth Factor (VEGF) and therefore are called anti-VEGF agents.
Fluorescein Angiography – is a common, office-based diagnostic test that can help distinguish between wet and dry AMD. Fluorescein Angiography is performed by injecting sodium fluorescein dye into a peripheral vein with a small needle. The dye then travels through the blood vessels. Choroidal neovascularization – the sign of wet AMD – can be visualized as a leaking blood vessel complex under the retina. After the test, patients will experience some transient yellowish skin discoloration and orange urine. Most patients tolerate the test well but a small percentage experience nausea and very rarely will have an allergic reaction.
Optical Coherence Tomography (OCT) – is a quick non-invasive, office-based imaging technique that uses a low energy laser to scan the macula and create a detailed map of the retinal architecture. OCT can help determine if there is fluid inside or beneath the retina which may indicate wet AMD. It is a commonly used test to monitor the response to treatment of AMD and has no risk to the patient.
Color Photography – patients may undergo color photography of the retina to document drusen, pigment changes, hemorrhages and other characteristics of AMD.
An Amsler Grid is a checkerboard that may be used to monitor for any changes in the macula. One eye is tested at a time with your reading glasses (if necessary).
During the test, you should concentrate on the center black spot and examine the checkerboard with your side vision. All the squares should appear straight with no distortion or missing areas.
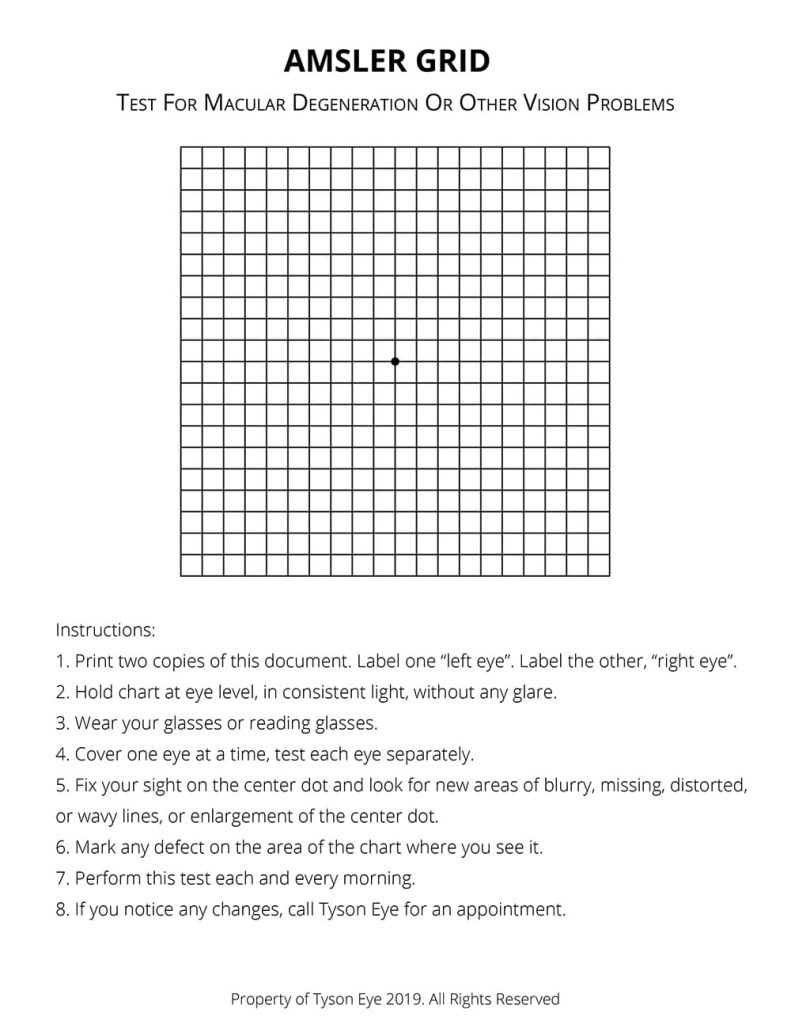
Any changes noted in the Amsler Grid should be reported to your eye doctor immediately.
Thermal laser photocoagulation may be used in certain, rare cases of choroidal neovascularization where the abnormal blood vessels are outside the center of the macula. Thermal laser treatment attempts to heat and destroy the abnormal blood vessels but will also damage the surrounding tissue. Therefore, this procedure is used less commonly given the advances with anti-VEGF agents.
To prepare for an injection, the eye is cleaned with antiseptic solutions and numbed with topical anesthetic gel or an injection of anesthetic into the eye. Injections are administered according to the patient’s response to treatment until the patient’s vision is stabilized and the leaking blood vessels have dried up. Ongoing treatment may be needed to control the disease.
The frequency and number of injections needed varies considerably among patients. The risks of intraocular injections include hemorrhage, retinal tear, and infection, all of which are very rare. The injection of steroid medications may increase the risk of cataract and elevated eye pressure (glaucoma).
Patients should call their doctor if they experience increased pain or decreased vision in the days following an injection as these symptoms could indicate a serious infection.
Most people with AMD will retain good central vision and the ability to read. This is because 90% of patients with AMD have the dry form that has a more favorable prognosis. Patients with wet AMD will suffer central vision loss if left untreated. However, the injection of anti-VEGF medications can improve the prognosis. More than 70% of patients with wet AMD will maintain or have improved vision and more than one third patients with wet AMD will have significant visual improvement.
Need help? Reach out to us today at 239-542-2020.
The material contained on this site is for informational purposes only and is not intended to be a substitute for professional medical advice, diagnosis, or treatment.
Always seek the advice of your physician or the other qualified health care provider.